Is Dental Sleep Medicine Ready for PrimeTime?
Dental Sleep Medicine (DSM) appears promising: a growing patient population, unmet clinical needs, and a potential new revenue stream. But behind the opportunity lies a fragmented and immature business environment plagued by reimbursement uncertainty, regulatory inconsistencies, and market confusion.
This article briefly details the business challenges, opportunities, and risks involved in DSM for providers and commercial stakeholders
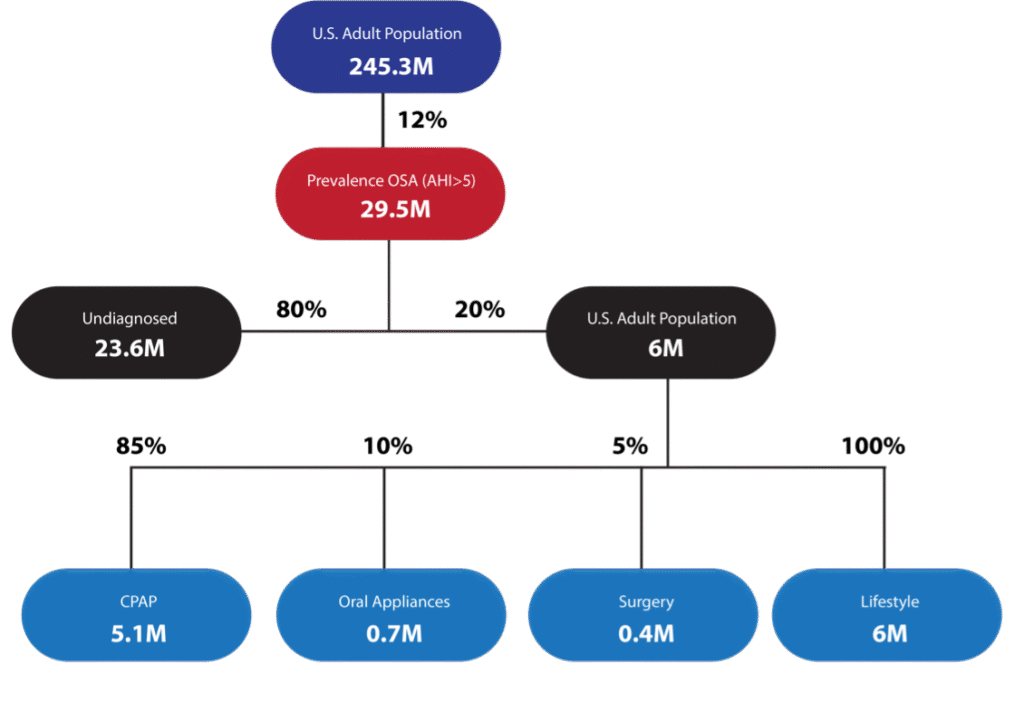
THE SCOPE AND COST OF OSA
Obstructive Sleep Apnea (OSA) affects roughly 30 million Americans, but 80% remain undiagnosed. Untreated OSA is linked to significantly increased risks of hypertension, diabetes, heart disease, stroke, and cognitive decline. Sleep deprivation is so serious that the Geneva Convention classifies it as torture.
OSA is diagnosed using the Apnea-Hypopnea Index (AHI), but that metric has flaws. Newer approaches like Mean Disease Alleviation (MDA) and hypoxic burden offer better insights into disease severity and overall treatment success.
The societal burden is staggering. In 2017, untreated OSA cost the U.S. $160 billion in lost productivity, healthcare utilization, and automobile and workplace accidents. In contrast, diagnosis and treatment costs totaled just $12.5 billion.
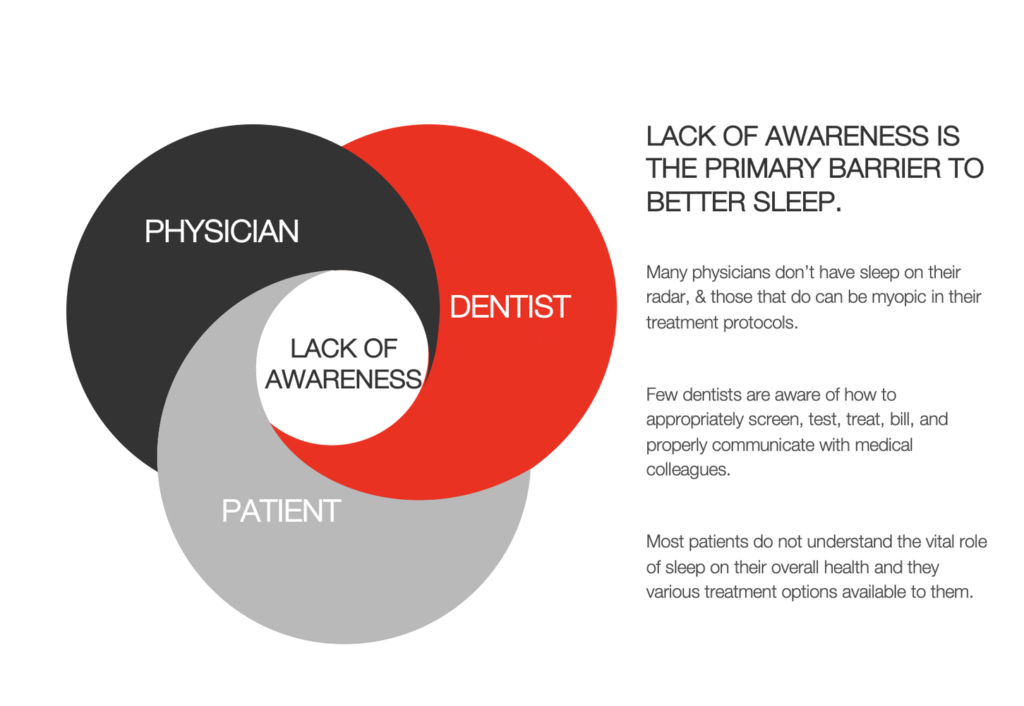
LACK OF AWARENESS IS PUBLIC ENEMY #1
The #1 problem DSM faces involves awareness, more specifically, the lack of it.
Jill and Joe Public don’t know what sleep apnea is. They don’t understand how it impacts their overall health. If the Publics do know anything about it—perhaps they’ve been diagnosed—it’s almost guaranteed that they lack awareness of OAT as a treatment option. In one recent survey, 76% of patients diagnosed with OSA had no knowledge of OAT.
Most physicians don’t know have sleep on their radar. Those that do are unaware that OAT exists as an effective, affordable treatment option for many patients. They don’t know who to refer patients to for OAT.
And the majority of dentists don’t know how to appropriately screen, test, treat, or bill for OAT. The ADA reports more than 200,000 dentists licensed in the U.S. but less than 1,300 dentists currently meet requirements as Diplomates of the ABDSM. Dentistry is a massive untapped workforce, but more motivation is required to attract dentists to this field. Increasing awareness, predictable reimbursement schedules, and establishing a more collaborative workflow between physicians and dentists are necessary steps to getting more patients into the proper diagnostic and therapeutic funnels.
WHO’S RESPONSIBLE FOR DIAGNOSING OSA?
With only 7,500 sleep physicians nationwide, access is limited. Meanwhile, more than 200,000 U.S. dentists are in prime positions to identify risk, but only 1200 are Diplomates of the American Board of Dental Sleep Medicine.
Most physicians and dentists don’t ask about sleep. Patients don’t connect symptoms like fatigue, brain fog, or weight gain with sleep disorders. Education and awareness are minimal.
DSM is an untapped opportunity, but a lack of training, collaboration, and reimbursement make it a minefield for most dental teams.
DIAGNOSIS: ROADBLOCKS AHEAD
OSA diagnosis requires a sleep test, either in-lab or at home. Dentists providing access to Home Sleep Tests (HST) use one of three pathways:
- Refer to a physician for testing (low cost, low patient return rate).
- Dispense in-house HST units (higher control, upfront investment).
- Use third-party HST providers (low cost, variable service quality).
The regulatory landscape is inconsistent. A few states still prohibit dentists from ordering HSTs. Others remain silent. The ADA, AADSM, and AASM all issue conflicting guidance. Medicare disallows dentist-ordered HSTs. Most private payors follow Medicare’s lead.
The ambiguity drives many dentists to avoid DSM altogether. But that shouldn’t be your fate.
TREATMENT LANDSCAPE
An increasing number of viable OSA treatment categories exist:
- CPAP – The current “gold standard.” Highly effective but poorly tolerated. Long-term adherence drops below 40%.
- Surgery – UPPP, MMA, and Inspire implants offer success but come with risks, high costs, and narrow indications.
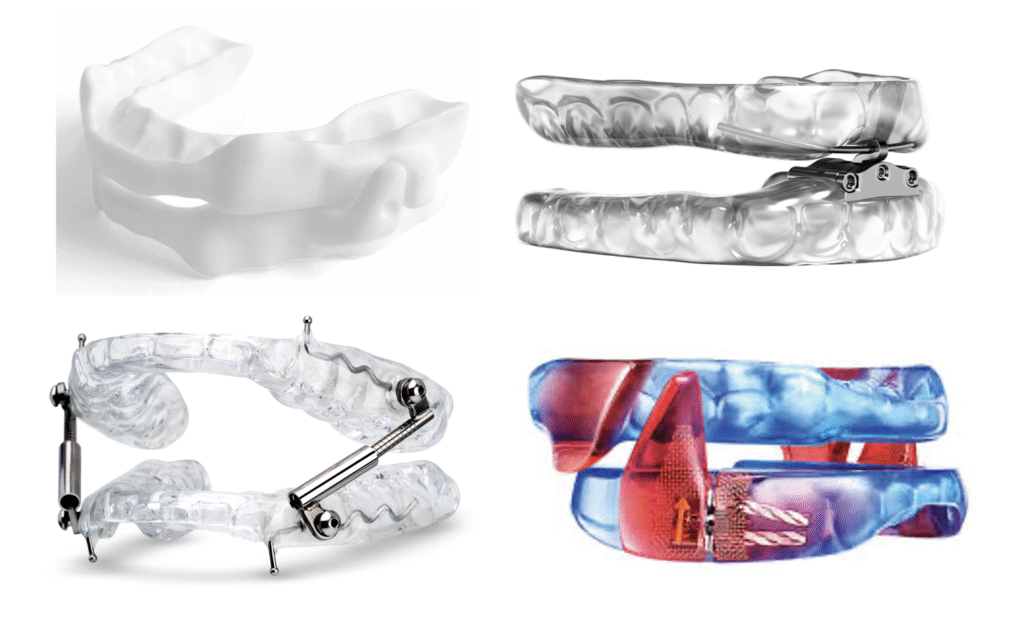
- Oral Appliance Therapy (OAT) – Delivered by dentists, these devices are effective, less invasive, and FDA-cleared. Yet OAT makes up just 7–10% of all OSA therapy. In attempts to increase OAT adoption, direct-to-consumer OAT companies are emerging, and an increasing number of ENT specialists provide OAT to their patients.
- Lifestyle Changes – Important but often insufficient alone and compliance is varied.
- Trizepatide – A major breakthrough and excellent co-therapy along with OAT, this injectable drug was previously approved for weight loss and diabetes management an is now FDA-approved for the treatment of OSA.
Recent events have shifted the landscape: A 2021 CMS report found CPAP has limited real-world impact on health outcomes. The Philips CPAP recall impacted 4 million users. Inspire has spent a third world country’s GDP on marketing their OSA solutions of which many interested patients are precluded. These developments threw open the window of opportunity for OAT growth. Sounds promising, huh?
DSM WORKFLOW: SCREENING, TESTING, TREATING, BILLING
Most practices offering OAT do not treat a high volume of patients resulting in each time being like the first time. It’s akin to visiting the gym one per month. You have to get the reps in to identify what’s working and figure out better ways for what isn’t working. The inefficient non-standardized workflow is like the snake that eats its own tail resulting in dentists bailing on this potentially life-saving procedure that can be crazy profitable for focused DSM practices.
Screening: Most dentists don’t screen for OSA, citing time constraints. But validated screeners take under 2 minutes. Screening is low-effort, high-impact, and underutilized.
Testing: Three models exist: referral to MDs, in-house testing, or third-party coordination. Each has benefits and risks. Dentists struggle to build referral relationships, explain the value of testing, and navigate compliance issues. Communication and consultative skills are often the missing links.
Treating: Over 150 FDA-cleared oral appliances exist. Most successful providers use 5–6. Yet analysis paralysis, low case volume, and a flood of conflicting CE courses stall adoption. Less than 1% of dentists treat 10+ sleep patients per year.
Billing: OAT isn’t covered by dental insurance. It requires medical billing which is a foreign concept to most dentists. Third-party billers fill the gap, but competency and communication varies. Reimbursement is declining, and bureaucracy is increasing. Many practices stagnate or abandon DSM altogether due to billing complexity.
I know several dentists whose practices collect over $5mn in OAT each year. They’ve risen to these challenges, overcome them, prospered, and profited. What are you gonna do?
IS DSM A GOOD BUSINESS?
For most, no.
Sadly, that’s the truth.
A few elite practices collect $1M+ per year in DSM. And there are a few that produce many multiples of that. But they are exceptions. Most dentists dabble and then quit. Volatility in billing, regulatory battles, and the uniqueness of treatment workflows make DSM unattractive to DSOs, investors, or large firms which emphasize standardization.
Big players in the dental field have tried and failed to make DSM a meaningful part of their businesses: Patterson, Henry Schein, Dentsply Sirona, Kavo Kerr. Glidewell uses DSM as a funnel, not a profit center. For others, the ROI in a nascent field just isn’t there.
Direct-to-Consumer OAT companies view OAT as a blue ocean opportunity. Noting the public dissatisfaction with PAP therapy and the success of Inspire, they recognize a market ripe for disruption. These companies launch online marketing campaigns to attract patients into their respective funnels, and then use centralized remote management to provide treatment. They will probably succeed. Will you?
YOU’RE IN THE GOLDEN AGE OF OAT—TIME FOR SOME ACTION!
DSM has so much potential, and it’s just about ready for prime time. The barriers are still high, but a growing number of dedicated providers have proven that you can do this.
And you should do this.
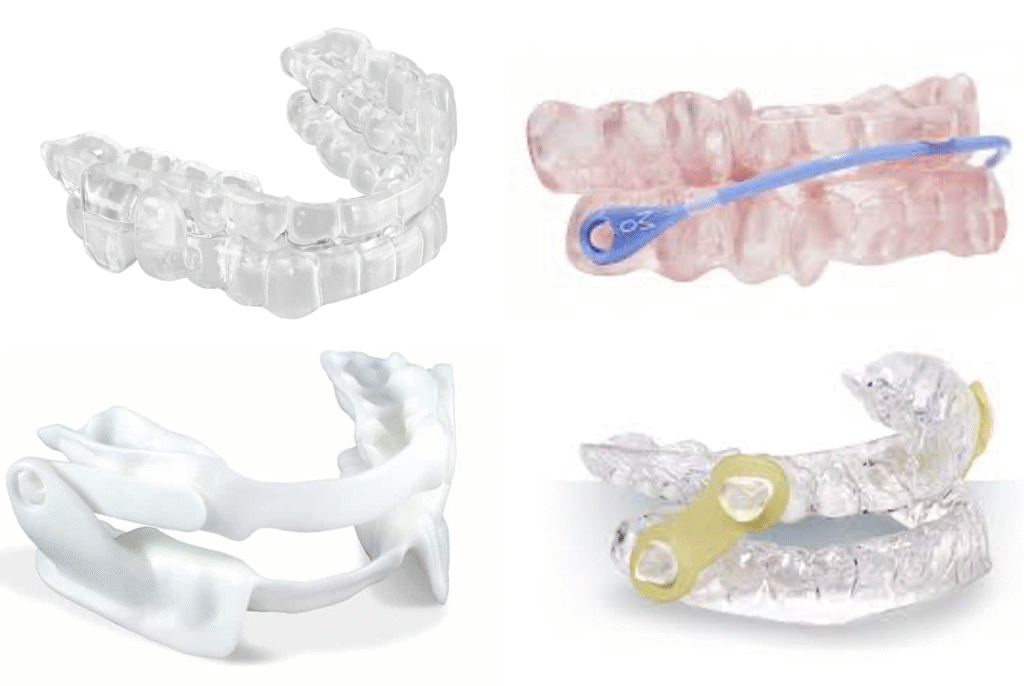
There have been numerous innovations in device design, manufacturing processes, and the quality of materials used for oral appliances. Precision medical devices are the name of the game.
The amount of high quality research supporting the effectiveness of oral appliances can fill a big-ass hard drive. A growing segment of the medical community is warming up to oral appliances as a desirable treatment modality for their patient populations.
There are more DSM education opportunities on any given weekend than there were in an entire year a decade ago – and some of that education is actually REALLY, REALLY GOOD.
Still, oral appliance adoption doesn’t even register as a blip on the actual OSA patient population radar. The onus is on all of us to direct Dental Sleep Medicine as a profession with real potential to seismically shift the sleep landscape. More than any time in the past, the future’s so bright, I gotta wear shades. There’s a race to bring oral appliances embedded with remote patient monitoring technology to market. This could be a decisive leveler in the OSA treatment field.
The aforementioned developments are compounding into REAL CHANGE. This is leading to more dentists getting involved and doing so with greater penetration. If you look at the customer reports from your favorite appliance manufacturers, you’ll see they have more clients than ever before and more of them are producing higher volumes of cases. In the parlance of the labs, there are less dentists doing onsies and twosies and more doing five to ten cases per month.
Get educated. Get a coach, a sleep champ, and a 3rd party biller. Get some cojones. And get going. The most successful practices were created by professionals that made conscious decisions to make it happen. They didn’t wait for the regulatory and payor stars to align. They made their futures.
If they did it, you can do it too. Hire a competent third party billing company. Designate someone as your SLEEP CHAMPION and then educate them, equip them with the resources they need to do the job, empower them to do it, and encourage them. Reward wins & coach when the goal is missed.
- Generate a vision.
- Outline the path forward.
- Delegate appropriately.
- Execute – don’t let your sleep dreams die by analysis paralysis.
- Evaluate what’s working and what isn’t.
- Then pivot as warranted.
Take action. Again. And again.
Lobby the American Academy of Dental Sleep Medicine to step up and advocate for the profession.
Consider reading this book, too.
Your patients, your practice, and the DSM profession will benefit.

Your Company’s Future Is a Real Page Turner!
I like to read. Books. In conversations with others, I’ve…
3 Business Lessons Learned from Watching the Tiger King
Like bazillions of Americans, last week I was shamefully glued…
