From fat-shaming to carnivore-shaming, shame has been, well, shamed over the past decade. Shaming someone for behavior once deemed inappropriate is viewed as more reprehensible than the actual act. Many behaviors and lifestyles that were the targets of scorn and shaming a generation ago are now celebrated in a culture that is increasingly tolerant.
Research published in Social Forces has shown that over the past 40 years, American tolerance has increased. “The increase in tolerance is positively correlated with higher levels of education and individualistic attitudes, including rejecting traditional social rules…” These favorable shifts are a reflection of cultural enlightenment. However, I suggest you not throw out the baby with the bath salts.
has shown that over the past 40 years, American tolerance has increased. “The increase in tolerance is positively correlated with higher levels of education and individualistic attitudes, including rejecting traditional social rules…” These favorable shifts are a reflection of cultural enlightenment. However, I suggest you not throw out the baby with the bath salts.
Shame effectuates societal norms. Sure, cutting off thieves’ hands reduces the likelihood they’ll physically be able to swipe a carload of handbags, but maybe more important, it serves as a shameful reminder to all and forever brands him with the shame of stealing from others. This is especially damning when in a smaller community.
 I’m not advocating Taliban-style tactics. I am suggesting that we take a look at the powerful, persuasive, positive aspects of shame. It is in these localized groups that shaming someone for violating normative behaviors can have the greatest effect on transforming attitudes and changing behaviors. Let’s try an exercise. If you could save my life but chose not to do so because you were unsure how much insurance would pay you, what does that say about you?
I’m not advocating Taliban-style tactics. I am suggesting that we take a look at the powerful, persuasive, positive aspects of shame. It is in these localized groups that shaming someone for violating normative behaviors can have the greatest effect on transforming attitudes and changing behaviors. Let’s try an exercise. If you could save my life but chose not to do so because you were unsure how much insurance would pay you, what does that say about you?
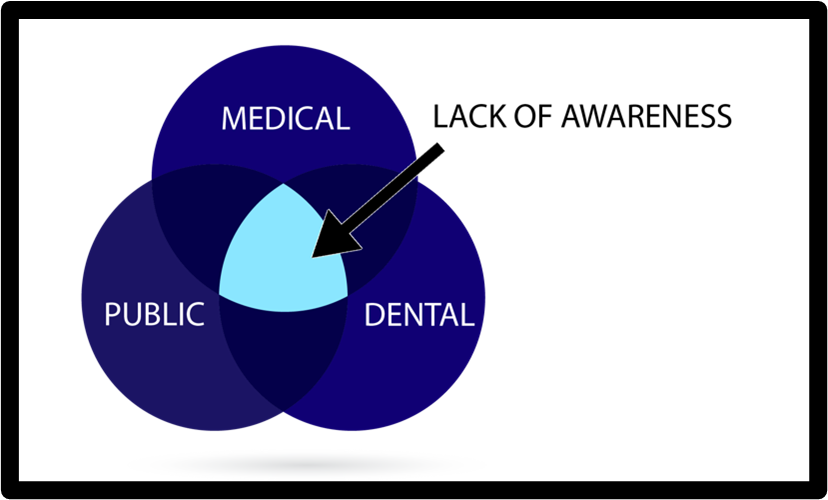
If you possess the ability to potentially save patients’ lives but you don’t, are you ethical or unethical or does that fall into some gray area? Is it unethical if you, as a dentist, choose not to screen for obstructive sleep apnea (OSA)? The ADA says you should screen at the very least. So does the AADSM.
What if I was in your practice for a prophy yesterday and despite being a 48 year-old male with a big-ass tongue and signs of extreme bruxism, no one talked to me about OSA – and then tonight I die from a heart attack?
I was a guest on a podcast a few weeks ago where an MD inferred that sleep physicians prescribing CPAP for mild & moderate OSA are moonwalking the malpractice line because they know more desirable solutions such as oral appliance therapy exist.

Today you might justify the decision not to screen patients for OSA by claiming that your practice is too busy, or the treatment pathways are convoluted. What if litigation follows and the lawyers produce the standards I mentioned earlier? What happens then?
Maybe you’re thinking that it dental sleep medicine isn’t profitable. There are a few dental sleep practices collecting 8 figures each year and many others are annually in the 7 figures. Can this help your business? As Benjamin Franklin stated, you can “…do well by doing good.”
Then why aren’t you doing it? Why are you postponing best practice, ethical action, and business growth? Screening your dental patients for OSA doesn’t just help them sleep better at night. It helps you sleep better at night, too. If you’re not doing it, shame on you.



 I’m not advocating Taliban-style tactics. I am suggesting that we take a look at the powerful, persuasive, positive aspects of shame. It is in these localized groups that shaming someone for violating normative behaviors can have the greatest effect on transforming attitudes and changing behaviors. Let’s try an exercise. If you could save my life but chose not to do so because you were unsure how much insurance would pay you, what does that say about you?
I’m not advocating Taliban-style tactics. I am suggesting that we take a look at the powerful, persuasive, positive aspects of shame. It is in these localized groups that shaming someone for violating normative behaviors can have the greatest effect on transforming attitudes and changing behaviors. Let’s try an exercise. If you could save my life but chose not to do so because you were unsure how much insurance would pay you, what does that say about you?